2026 caregiver burnout statistics: How stress shows up in family caregiving
Lifestyle

Audio By Carbonatix
12:30 PM on Tuesday, February 17
By Susanna Guzman for A Place for Mom, Stacker
2026 caregiver burnout statistics: How stress shows up in family caregiving
Caregiver burnout is widespread, recurring, and closely tied to the realities of family caregiving rather than isolated moments of stress. Drawing on new 2025 survey data from A Place for Mom, this report examines how stress and burnout manifest across emotional, physical, social, and financial dimensions, as well as the caregiving conditions that shape them.
Burnout is widespread and recurring
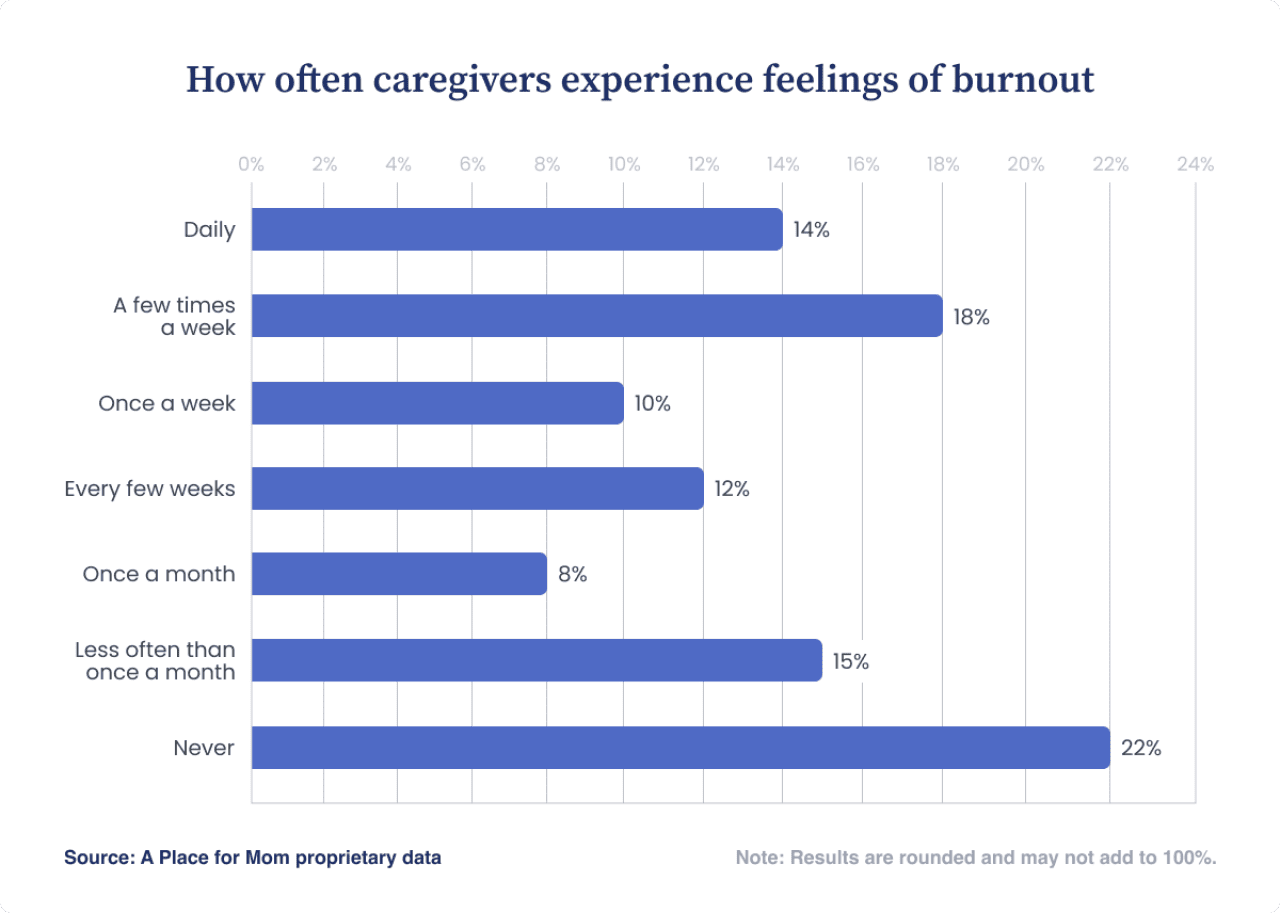
More than three-quarters of caregivers experience feelings of burnout, with many describing it as a weekly or even daily occurrence. Rather than appearing sporadically, burnout is often persistent, reflecting sustained pressure over time and the broader caregiving conditions in which it occurs.
Caregiver stress rarely appears in isolation
Burnout frequently overlaps with other forms of strain. Caregivers who report burnout also commonly experience emotional stress, disrupted sleep, changes in social connection, and financial pressure, underscoring that stress often spans multiple areas of daily life at once.
Early conditions shape caregiving stress
Preparedness and urgency play an important role at the outset of caregiving. Only about 1 in 4 caregivers report feeling completely prepared when caregiving began, and separate A Place for Mom data shows that urgent care needs and planning regret are common. These early conditions — limited preparation paired with time pressure — often coincide with elevated stress.
Strain and adaptation often coexist
Caregiving experiences are not uniform. Despite high levels of stress, many caregivers report confidence managing responsibilities, regular self-care, and stable or improved family relationships. This coexistence highlights a central tension in family caregiving: Strain and adaptation frequently appear together rather than canceling each other out.
How caregiver stress shows up in family caregiving
Caregiver burnout is widespread in the U.S., but it’s only one aspect of caregiver stress. In A Place for Mom’s 2025 caregiver survey, 78% of caregivers report experiencing feelings of burnout, with many describing burnout as a weekly or even daily occurrence. Beyond burnout, caregivers also experience emotional, physical, social, and financial impacts related to their role. These findings are aligned to those published by the World Health Organization in its report on family caregiving and public health.
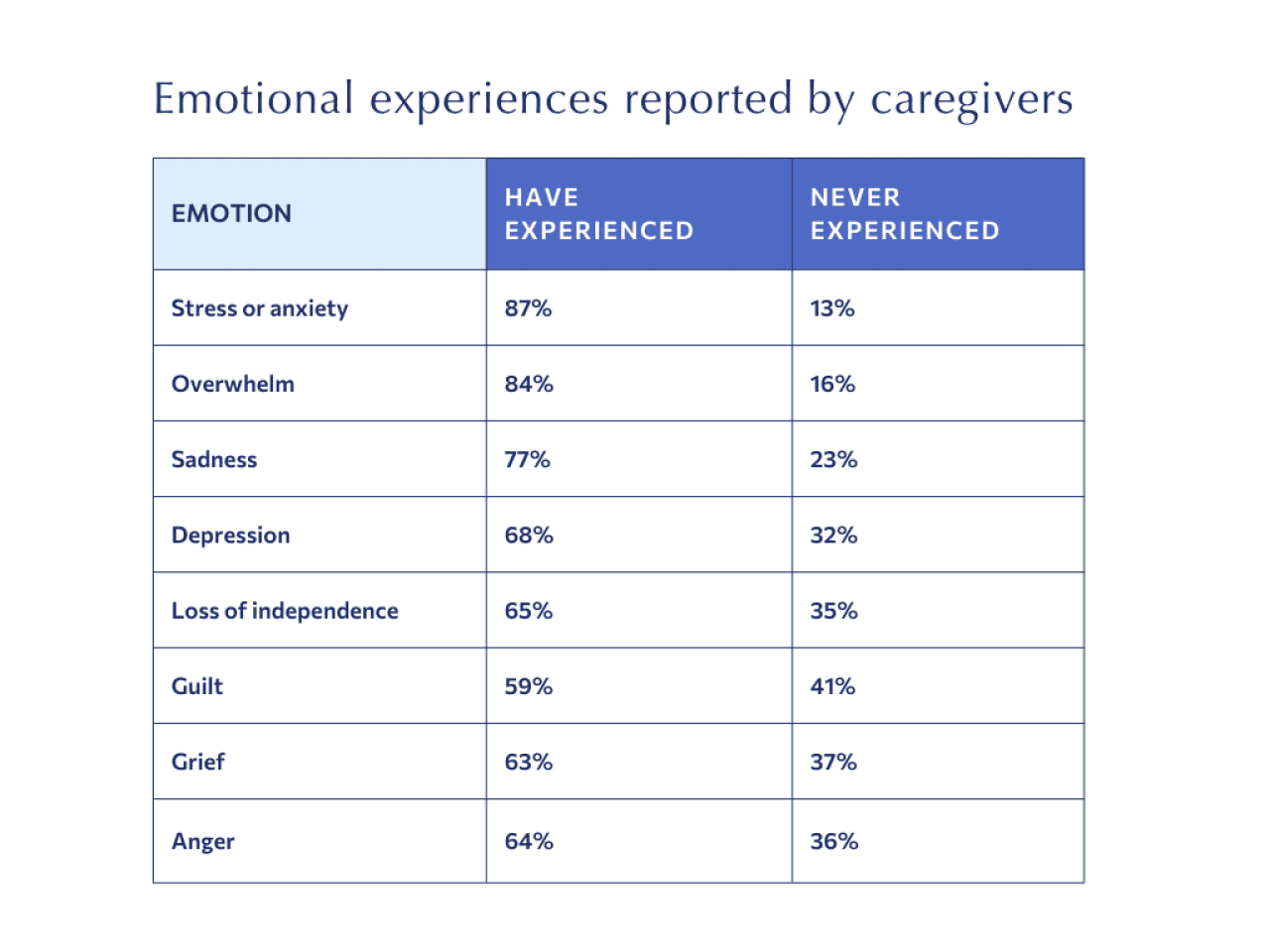
Emotionally
The survey data shows that many caregivers experience a broad range of emotional challenges, often as recurring parts of daily life. Stress and anxiety are the most prevalent, reported by 87% of caregivers at some point and experienced at least weekly by more than half. Feelings of overwhelm are almost as common, with 84% reporting it overall and nearly half experiencing it weekly.
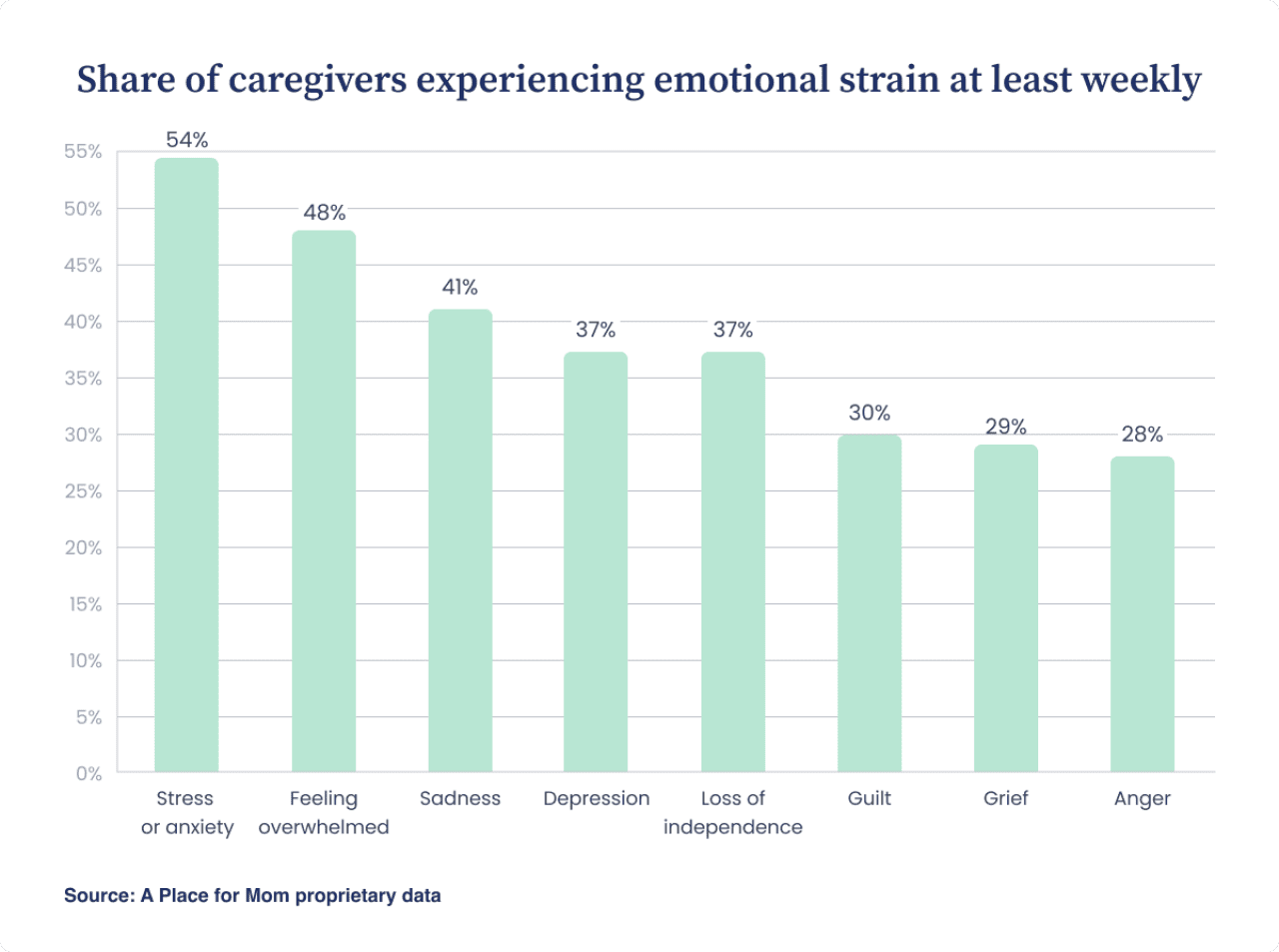
About 2 in 5 caregivers report feeling sad at least weekly, and more than one-third report recurring feelings of depression or a loss of independence. By contrast, emotions such as guilt, grief, and anger tend to surface less frequently, with roughly 3 in 10 caregivers experiencing them weekly. This distribution suggests that emotional strain among caregivers is variable rather than uniform, marked by persistent stress and overwhelm alongside other emotions that rise and fall over time. Even emotions that surface less frequently are experienced by most caregivers at some point.
That complexity is also reflected in how caregivers assess their overall mental health. When asked how caregiving has affected them, one-third said their mental health had worsened, while another third reported no change, underscoring that emotional strain can coexist with stability rather than following a single trajectory.
Physically
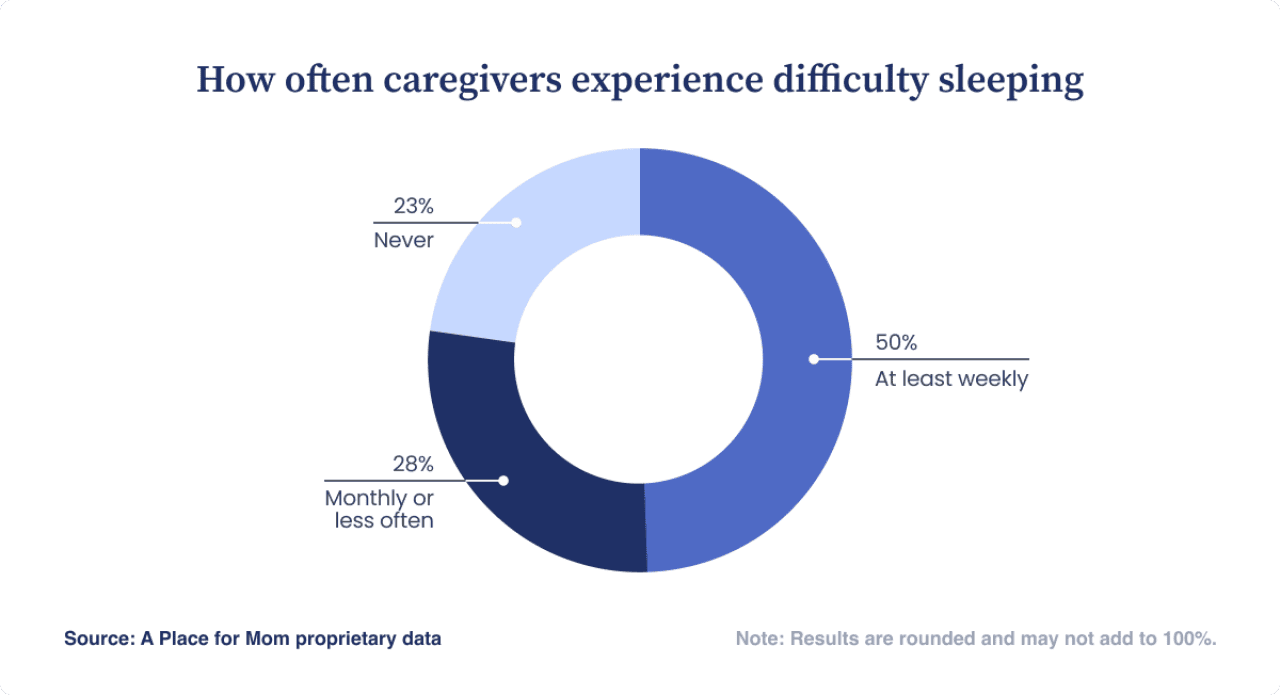
Caregivers paint a complex picture of their overall physical health and describe both positive and negative changes resulting from their caregiving role. One-quarter say that their physical health has gotten worse, 32% say it has improved, and 43% say it hasn’t changed.
Sleep stood out as a frequent challenge: One-half of caregivers report having trouble sleeping at least once a week. Peer-reviewed research supports treating sleep as a meaningful marker of overall health risk and suggests the sleep-health relationship often runs both ways.
Socially
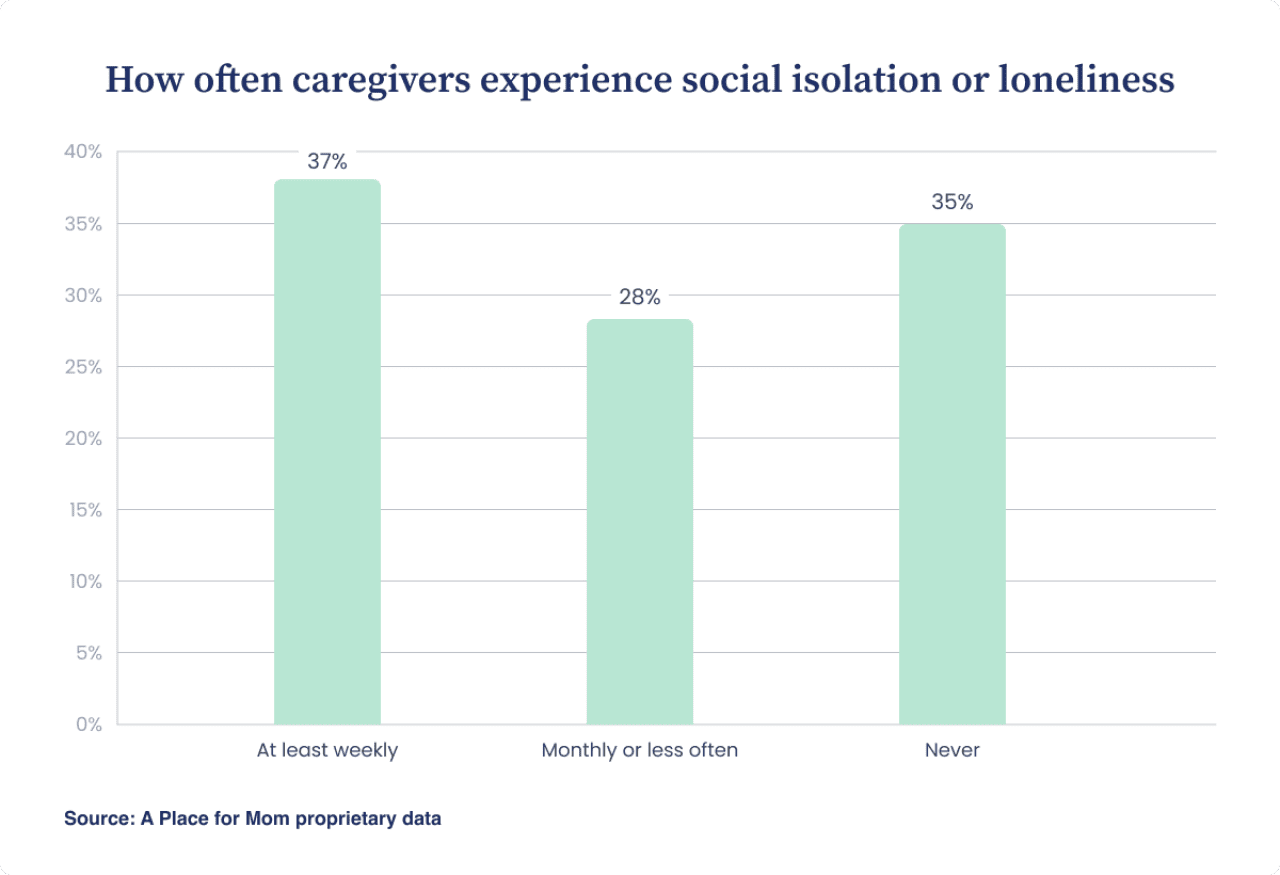
Feeling lonely and isolated at least once a week is common among family caregivers, and nearly 40% report that their social life has become worse after taking on caregiving responsibilities. That said, just over 60% say their social life has improved or hasn’t changed at all.
Financially
Financial experiences were mixed among the caregivers we surveyed, reflecting both stability and strain. Nearly two-thirds of caregivers (64%) say that caregiving has not affected their financial situation or has coincided with improvement, while 36% report that their financial situation has worsened.
Even among caregivers whose finances have remained stable, many report feeling financial pressure related to caregiving.
Of the family caregivers who responded to this survey:
- 32% say they aren’t experiencing any financial strain at all.
- 68% say that caregiving has created at least some financial strain.
These findings help explain why financial concerns can add to caregiver stress even when caregivers remain highly motivated and committed to their loved one’s care. The connection between financial strain and caregiver well-being is supported by peer-reviewed research.
The caregiving conditions that amplify stress and burnout
Daily caregiving experiences are influenced by more than what happens moment to moment. To understand why stress and strain feel more manageable for some caregivers and more overwhelming for others, it’s important to consider the broader caregiving context in which these experiences occur.
In the survey data, limited information and time to prepare, competing work and family responsibilities, and long-term or high-intensity caregiving frequently appear alongside stabilizing factors such as confidence, self-care, and family support. Together, these conditions help explain why caregiving experiences vary so widely, even among people providing similar types of care.
Limited preparation and urgent needs add pressure early in the journey
Most caregivers (70%) report beginning caregiving with some level of readiness, while 30% report feeling mostly or completely unprepared. These data illustrate that preparedness at the start of caregiving is often partial rather than complete.
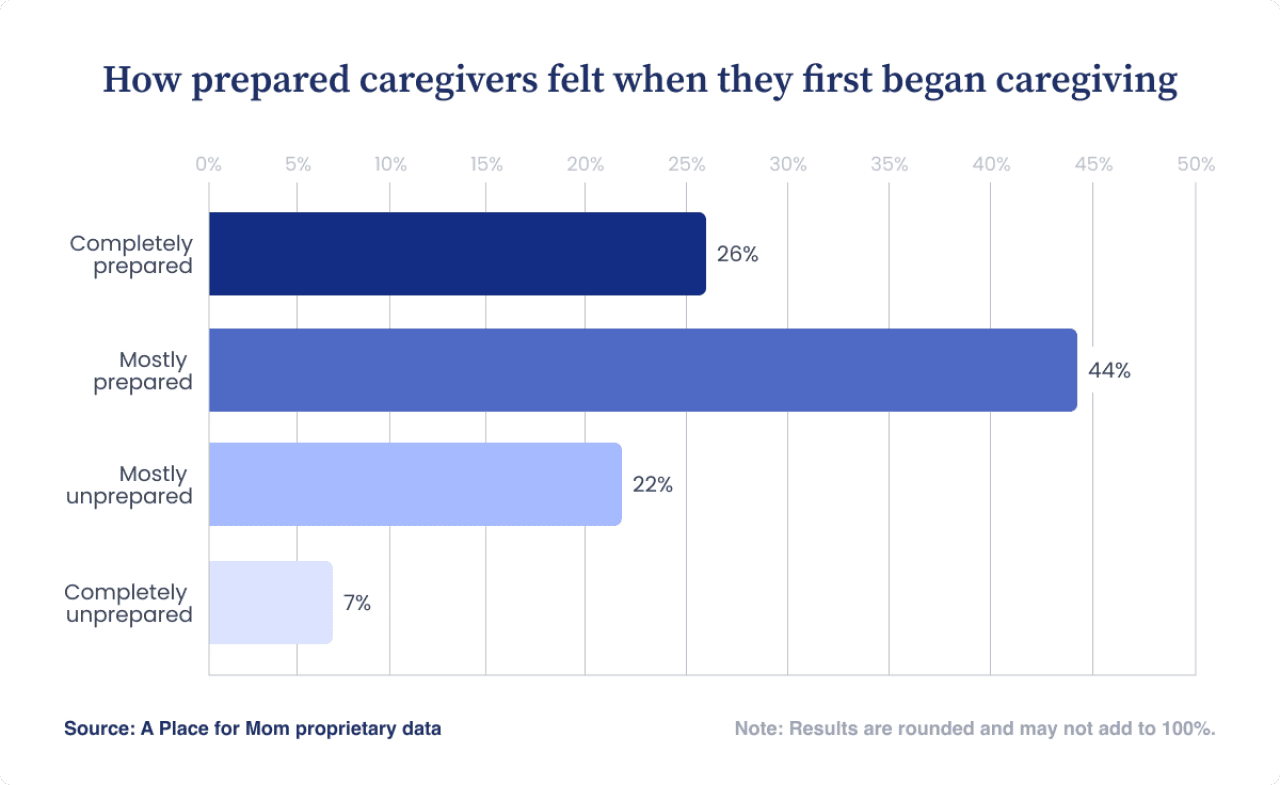
A Place for Mom’s 2025 Senior Care Search Trends Report sheds light on a related but distinct factor: the urgency of care needs. In that survey, caregiver responses show how frequently families face tight timelines and retrospective planning regret:
- 24% of caregivers who found senior care in the past year said their need was immediate.
- 25% of caregivers who found senior care said they needed care within 30 days.
- 54% of all caregivers surveyed said they wish they had started making a senior care plan sooner.
Together, these findings highlight two conditions that often coincide at the start of caregiving: limited preparedness and urgent need. Peer-reviewed research further notes that the transition into caregiving, when new care and logistical pressures increase at the same time, is commonly associated with heightened pressure, providing broader context for why caregiving, especially in the early stages, is frequently described as demanding.
Caregiving is often intense and long-lasting
Caregiving frequently requires significant and sustained commitments. In the survey, caregivers report spending an average of 22.8 hours per week providing care, and nearly 30% say they spend more than 30 hours per week on caregiving responsibilities. Duration is also substantial: 25% of caregivers report providing care for more than five years, and 75% say they have been caregivers for at least one year.
Peer-reviewed longitudinal research provides additional context for these patterns. A 2024 analysis identified “tipping points” at higher levels of caregiving intensity, where greater time demands are associated with lower psychological well-being over time. Together, the survey data and research findings highlight how caregiving often extends beyond short-term support and involves sustained demands.
Competing responsibilities are common
Many family caregivers are balancing work and caregiving, with 64% reporting that they also have full- or part-time jobs in addition to caring for elderly loved ones. Nearly one-half are members of the sandwich generation, a group of adults also caring for children or grandchildren under 18.
These findings show that caregiving often represents an addition to existing work and family responsibilities. While the survey didn’t measure how caregivers allocate time across their different roles, the overlap in responsibilities itself highlights why caregiving can feel difficult to compartmentalize and why strain may persist even when caregivers report confidence or motivation.
Factors that may buffer caregiver stress
Even within similar caregiving environments, day-to-day experiences can differ widely. Elements such as how responsibilities are shared within the family, how confident they are juggling multiple demands, and whether they practice active self-care can influence whether caregiving feels more manageable or more demanding over time.
Self-care and confidence
Many caregivers actively engage in self-care behaviors, such as exercise, socializing, hobbies, mindfulness, therapy, and creative activities, even while experiencing stress or strain. Nearly three-quarters (72%) report making time for self-care at least weekly and 58% report making time for self-care daily or a few times a week.
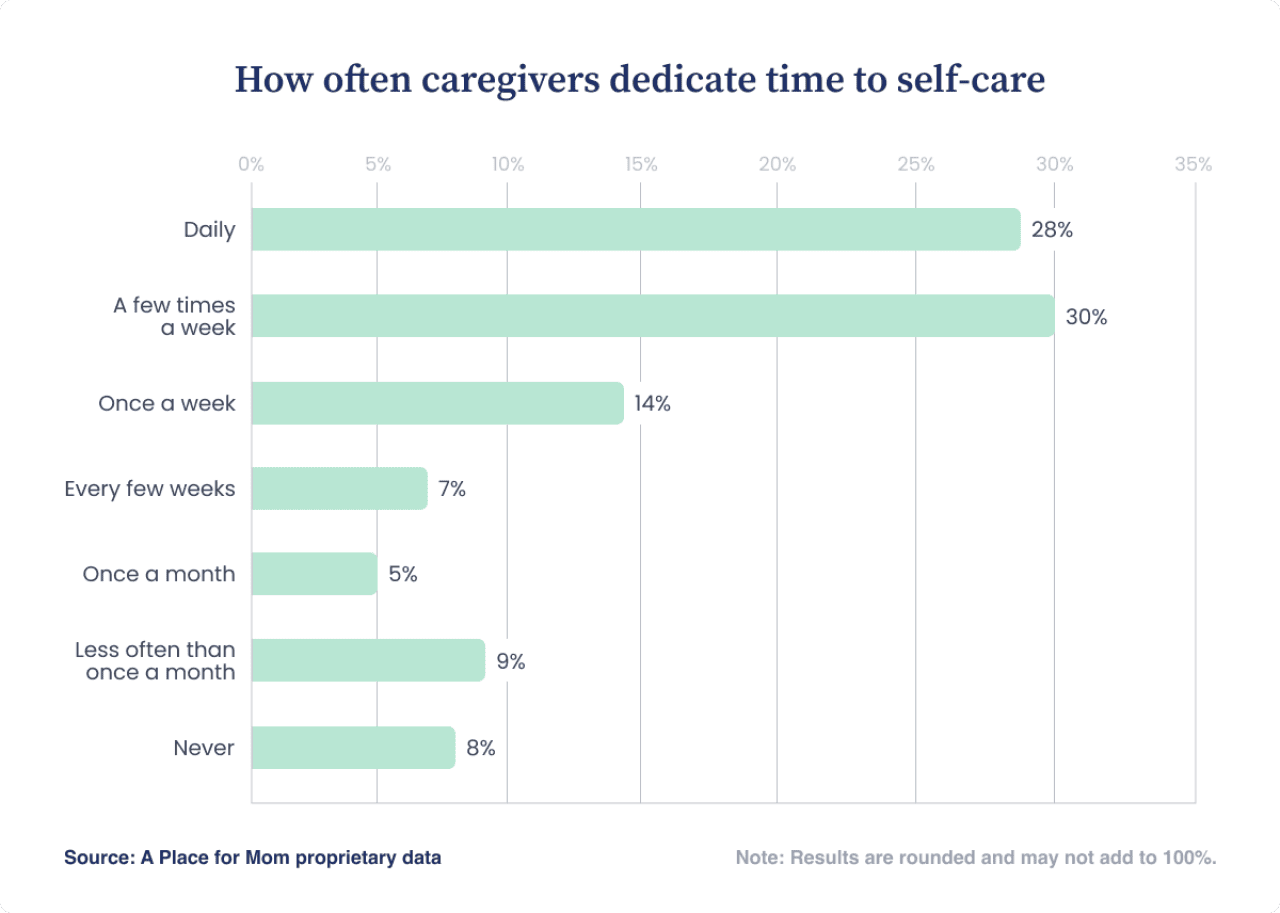
Confidence is also common among caregivers, even when stress is present. Nearly 98% say they feel at least some degree of confidence managing caregiving alongside other responsibilities, suggesting that strain and self-assurance often coexist rather than cancel each other out.
Family relationships
According to the family caregivers we surveyed, caregiving can deepen connection, meaning, or closeness for some families, even as it introduces strain. When asked about the impact of their caregiving role on family relationships:
- 45% say their relationships have improved.
- 42% say their relationships haven’t changed.
- 13% say their relationships have gotten worse.
These balanced results illustrate that family support can act as a buffer, while conflict or misalignment can add another layer of strain.
What these findings suggest about caregiving support
This report shows that caregiving in the U.S. is neither uniformly bleak nor quietly manageable. Many caregivers demonstrate adaptation, confidence, and commitment, yet the data also reveals a strong and persistent sense of overwhelm that cuts across daily life, long-term responsibilities, and major decisions. This tension raises deeper questions about how caregiving is structured, supported, and sustained, and who bears the cost when it isn’t.
Methodology
Except where noted, this report is based on an online quantitative survey commissioned by A Place for Mom and conducted by Morning Light Strategy in September 2025. The study included 1,029 surveys of a representative sample of family caregivers across the United States.
To contextualize these survey findings, we consulted selected peer-reviewed studies that examine mental and physical health indicators, social well-being, and caregiving context such as intensity, preparedness, and pressure to make decisions. These sources are used to compare patterns and alignment across data types, not to validate or “diagnose” burnout risk for any specific caregiver.
This story was produced by A Place for Mom and reviewed and distributed by Stacker.







